Genetic editing in humans, mRNA cancer treatments, surgeries planned via virtual reality. A few years ago, these medical breakthroughs would have belonged to science fiction. But they are just some of the very real technological advances reshaping the practice of medicine in the past year. As developments in biological research intersect with the exponentially expanding capabilities of AI and other technologies, we find our world on the cusp of a dramatic healthcare transformation.
While offering tremendous benefits for patients, these medical firsts also bring a slew of unknowns. What ethical questions must be confronted with the evolution of gene editing? Will animal organ transplants become the new normal? How might life-saving technologies be made equitably accessible?

With each new medical breakthrough, we find ourselves in remarkable, uncharted territory. These six advances of 2023 are both revolutionizing healthcare and inspiring us to think differently about medicine’s role in our world.
Organ Transplants from Animals and 3D Bioprinting
According to the U.S. Health Resources and Services Administration, 17 people die each day in the U.S. waiting for an organ transplant; and every ten minutes, another person is added to the transplant waiting list. Though over 130,000 organ transplants are performed globally each year, most people die waiting (over 6,000 in the U.S. annually), or never even make it onto the list.
In a highly experimental 2022 procedure, a genetically-edited pig’s heart was transplanted into a 57-year-old man named David Bennett by surgeons at the University of Maryland. (Experiencing end-stage heart failure, Bennett was not eligible for a traditional human organ transplant.)
Researchers had removed pig genes known to trigger a rapid rejection of the organ and added human genes to encourage Bennett’s body to accept the heart, but they had little idea of how his body might react.
Remarkably, he not only survived the transplant, but was able to live for two months with the pig’s heart in his chest. There are still leaps and bounds to be made in the technology—such as refining the process of genetically editing the organ to make it more compatible. But if animal organ transplantation, also known as xenotransplantation, evolves to become a viable clinical option, this practice could save hundreds of thousands of lives every year.

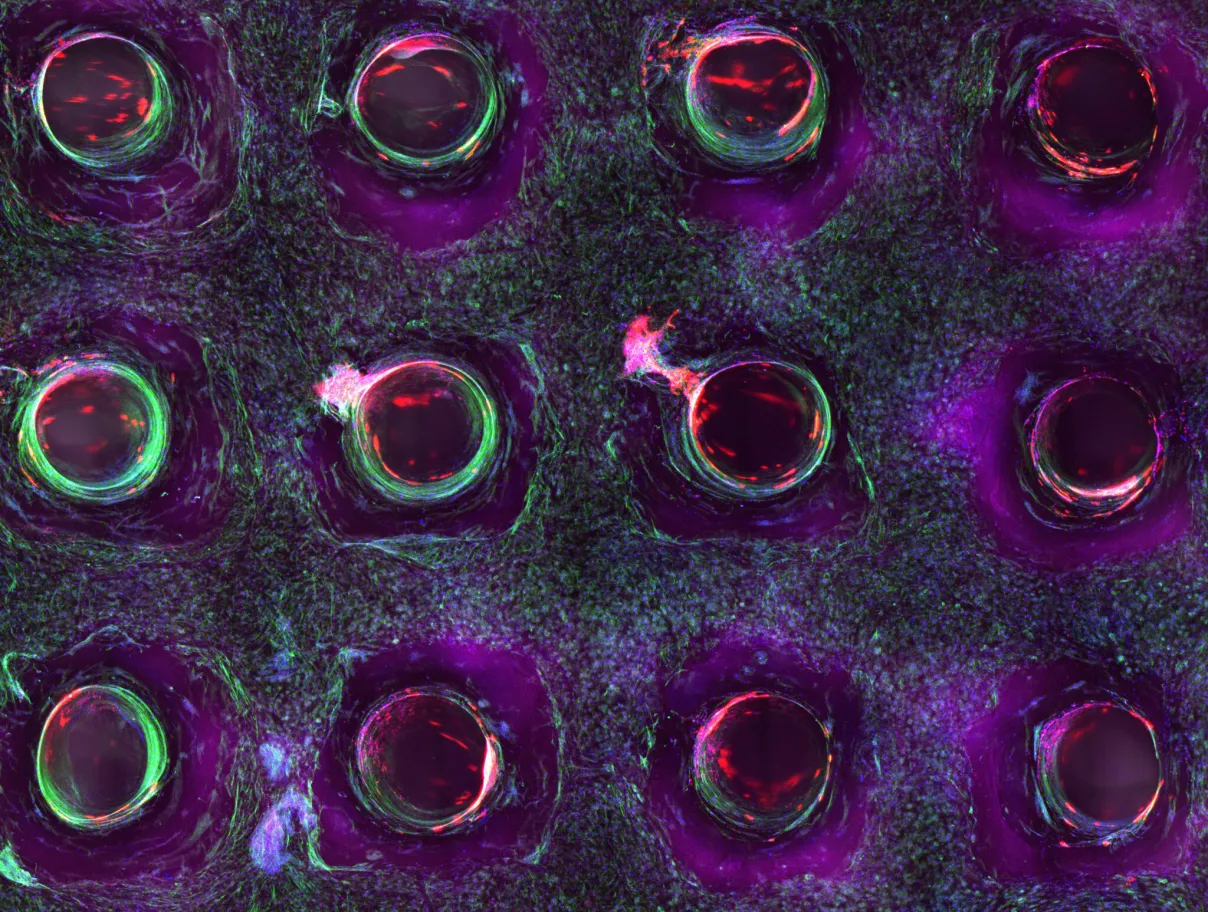
As a supplement, or maybe even an eventual alternative, to xenotransplantation, researchers have been working for the past number of years on developing our capacity to 3D print human tissues on silicon. The Wyss Institute, Harvard University’s center for biologically inspired engineering, has developed a method of 3D bioprinting human tissues that are able to function for upwards of six weeks.
Megan Laura McCain, Ph.D., associate professor of biomedical engineering at USC, explains that 3D bioprinting “can fill in a lot of knowledge gaps that cannot be addressed with conventional models.” This innovative approach is “especially valuable for studying diseases that are rare and/or human specific, which cannot be modeled in animals,” says Dr. McCain. “We can even make therapies tailored to the patient by using their own cells for testing.”
Though still in the earliest stages of development, both xenotransplantation and 3D-printed tissues have the remarkable capacity to save thousands of lives in the near future. “These systems will continue making real impacts,” says Dr. McCain.
mRNA Cancer Treatments
After the meteoric success of mRNA vaccinations for COVID-19, mRNA—the molecular template for protein production—was catapulted into the public spotlight. This type of vaccine technology works by providing the body with instructions on how to produce a disease-specific antigen, a marker that indicates a substance is dangerous to the body. It gives the immune system a head start on producing the proteins that fight a specific pathogen. While the success of mRNA vaccines against COVID-19 seemed sudden and remarkable, researchers have been developing this technique for 30 years.
Over the course of the past decade, research efforts have aimed to apply mRNA vaccine technologies to cancer treatment. This year, a National Institutes of Health (NIH) funded team from the Memorial Sloan Kettering Cancer Center (MSKCC) published the results of a clinical trial studying the efficacy of a personalized mRNA cancer vaccine for pancreatic cancer. Functioning similarly to the COVID-19 vaccine, its mRNA contains instructions for cells to stimulate an immune response against a specific abnormal protein present in tumor cells. This technique contrasts with other immunotherapies that stimulate the immune response generally instead of targeting a specific cancer, explained Patrick Ott, M.D. Ph.D., a clinical director at the Dana-Farber Cancer Institute, in an interview with the National Cancer Institute.
In the case of the MSKCC study, customized vaccines were created for each pancreatic cancer patient based on a gene sequencing of their individual tumors. According to the NIH, the process of creating and delivering each vaccine only took an average of nine weeks, an exceptionally fast production process made possible by the mRNA vaccine infrastructure established during the pandemic. Eighteen months into receiving these personalized mRNA treatments, the pancreatic cancer patients who had strong immunological responses to the vaccine were cancer free. On the other hand, patients whose immune systems didn’t respond to the vaccine (around half of the participant pool) had their cancers return within a year.
In a statement, Dr. Vinod Balachandran, head of the MSKCC team, said that such personalized vaccines may work to effectively treat other cancers, as well.
Virtual Reality in Surgery
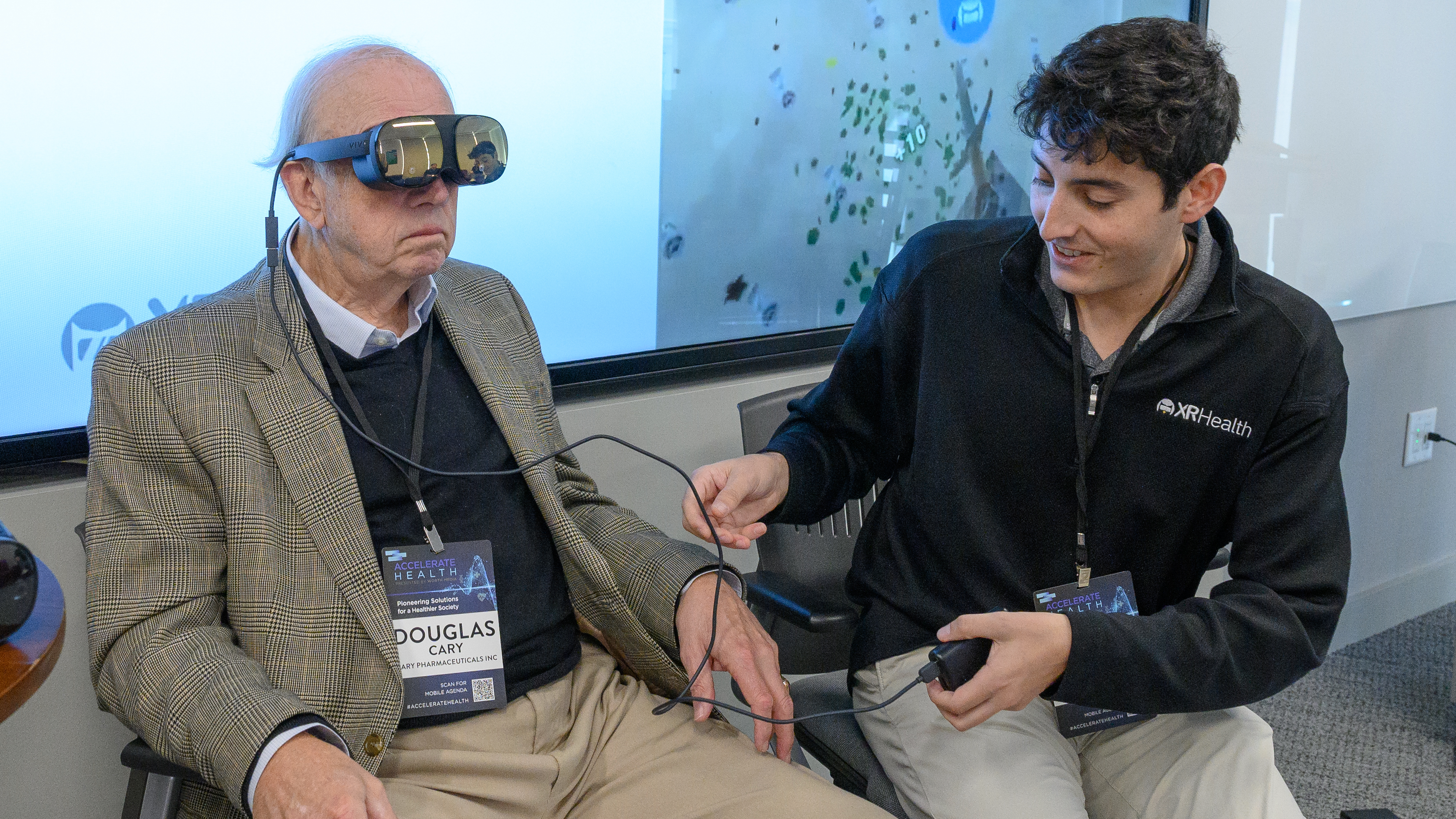
Once relegated to the realm of video games, the concept of augmented and virtual reality (VR) is rapidly gaining traction, particularly following recent initiatives from technology giants Meta and Apple. But unknown to most is the impact that virtual reality is having across the field of surgery. From being used as an exceptional teaching device to giving surgeons an unequaled visual preview to prepare for a complicated procedure, VR has become a powerful tool in surgical practice.
Typically, surgical training requires innumerable resources, immense logistical planning, and days-long workshops. VR fills a critical role in offering surgeons a robust training system. Not only can it be used to demonstrate and teach surgical techniques, but trainees can use VR to practice on their own. VR “can be used to help surgeons master new procedures,” says Thomas B. Talbot, MD, principal medical expert at the USC Institute for Creative Technologies.
A surgeon needs to perform at least 75 cases of a surgery to achieve optimal proficiency. “Virtual training allows for training an individual on an on-demand basis while allowing for repetition of an experience as many times as needed,” says Dr. Talbot. A clinical validation study from UCLA’s David Geffen School of Medicine found that VR training improved participants’ surgical performance by 230% in comparison with traditional training techniques. Virtual reality training platforms can further score surgical performance and proficiency, a qualitative measure that is incredibly valuable to ascertain competency in such a high-stakes discipline.
Like an F1 or flight simulator, virtual reality technologies can also help surgeons carefully plan for a procedure by allowing them to explore and understand a patient’s anatomy beforehand. By feeding more conventional 2D visualization tools such as an MRI or CT scan into a 3D model, VR grants doctors a comprehensive view into the human body. For instance, it helps surgeons understand how to address a tumor while steering clear of other critical and vulnerable areas in the brain, such as the motor cortex. VR also allows patients to gain a better understanding of their own surgeries. After being shown VR renderings of her aneurysm, a neurosurgery patient explained she felt reassured, knowing that the process was so straightforward.
This practice has also been employed in surgical oncology, particularly in procedures to remove masses or certain tumors in the lungs and chest. The 360-degree view helps surgeons to see exactly where a specific patient’s airways, organs, and blood vessels lie in relation to each other, thereby enabling doctors to ascertain whether a surgery can be performed safely. In addition to improving post-op outcomes, the detailed 3D visualization that VR provides may serve to avoid exploratory procedures that put patients at unnecessary risk.
Artificial Intelligence in Clinical Trials
From conducting appointments via Zoom to having participants administer treatments in the comfort of their own homes, clinical trials have become increasingly more streamlined over the course of the past few years. Further, the abnormally rapid process of creating a safe and effective COVID-19 vaccine has set a precedent for swifter clinical trials going forward. While researchers and pharmaceutical companies grapple with the pressures of producing safe and effective treatments on a tight timeline, many are turning to artificial intelligence and machine learning to expedite trial outcomes. Researchers in a 2023 statistical study of AI implementation across various clinical trials determined that the use of AI technologies can improve the probability of success, reduce labor, and speed up research and regulatory approval.
Patient recruitment is one of the most time-consuming and labor-intensive aspects of clinical trials and is essential to a trial’s efficacy. Instead of hiring various teams to sort through mountains of records—as well as contact, screen, and recruit potential trial participants—new machine learning models and algorithms can automate this process. Beyond that, AI works to rapidly aggregate and manage data from trial subjects across hundreds of geographical locations, proving to be an invaluable tool in facilitating database management, literature review, and analysis.
By implementing algorithms to build a trial’s foundational database, a process that can sometimes take ten weeks or more can be reduced to only one week with the help of AI. Once a trial is launched, AI is also able to expedite the process of sorting, cleaning, and analyzing results and can even flag unusual results for researchers to review, thereby saving hours of tedious labor. Moreover, data visualization is massively aided by the use of AI, including the generation of explanatory charts and graphs.
The cost savings from AI are especially valuable in clinical trials for treatments that don’t necessarily promise big profits and thus don’t attract much funding. This is often the case with rare diseases or targeted therapies, such as trastuzumab for HER2-expressing breast cancers.
CRISPR/Cas9 Gene for Heritable Diseases
The term CRISPR/Cas9, a precision DNA editing tool, has been a buzzword across the scientific community for over a decade. But since its introduction in 2012, CRISPR/Cas9 technology has improved and is now being experimentally applied in the treatment of heritable chronic diseases.
At this past spring’s Third International Summit on Human Genome Editing, an unlikely speaker took the podium: Mississippi native and Walmart cashier, Victoria Gray. As one of the first patients to receive an experimental CRISPR/Cas9 treatment for sickle cell disease, Gray spoke of her transformational experience with the groundbreaking procedure. “I really feel that I’m cured now,” she said. “I came from having to have an in-home caregiver to help me take baths, clean my house, and care for my children. Now I do all those things on my own.”
In sickle cell disease, abnormal hemoglobin from a very specific genetic mutation causes red blood cells to take on a crescent or “sickle” shape that clogs blood vessels. This impedes blood flow, leading to serious issues including anemia, bacterial infections, strokes, and episodes of extreme pain. The disease affects over 100,000 people in the United States alone; one in 13 African American babies carry the genetic trait.
In Gray’s experimental treatment, doctors used CRISPR/Cas9 to edit out the causal mutation in billions of her bone marrow cells. Once these amended bone marrow cells were injected back inside her body, they began to produce functional hemoglobin, capable of compensating for Gray’s otherwise defective hemoglobin.
CRISPR Therapeutics and Vertex Pharmaceuticals, the companies that funded the study Gray was a part of, have successfully used CRISPR/Cas9 to treat 75 patients with sickle cell disease or beta thalassemia, a related condition. The study (peer reviewed in the New England Journal of Medicine) found that after treatment, all of the sickle cell patients had been relieved of symptoms, despite having been diagnosed with severe cases of the illness. Based on their extraordinary results, the companies have submitted their treatment to the FDA for approval, a significant step towards making gene editing therapies broadly accessible.
However, CRISPR/Cas9’s broad gene-editing capabilities bring with them heavy ethical implications. The novelty of the technology means that researchers are uncertain of how long the benefits of treatment might last, or if patients might suffer unanticipated, long-term effects from the genetic-editing. What’s more, CRISPR/Cas9 therapy currently costs between $1.3 and $1.9 million to conduct per patient, raising equity concerns as to who will be able to access the life-changing treatment. The burden of sickle cell disease is disproportionately large in populations of sub-Saharan African descent. And many of the patients with the greatest need live in less affluent communities or nations that lack the facilities to perform such a complicated procedure.
Alzheimer’s Breakthroughs
Because of the incredibly complicated nature of Alzheimer’s disease, a catastrophic neurodegenerative illness, progress in developing treatments has been a slow and frustrating process. But over the course of this past year, researchers have made two critical breakthroughs in the treatment and understanding of the illness.
At the beginning of July, the FDA granted full approval to the drug Leqembi, the first Alzheimer’s medicine demonstrated to actually slow the progression of the pernicious disease—by about 27% after 18 months of treatment. Subsequently, the Centers for Medicare and Medicaid Services announced that they would expand their coverage to include the drug, a life-changing development for an estimated one million patients in the U.S. alone. Prior to the FDA’s official approval, Leqembi cost over $26,000 per year without insurance coverage. Though only those with early forms of the disease qualify for the treatment, the drug’s approval has the capacity to benefit over a sixth of Americans diagnosed with Alzheimer’s.
Characterized by amyloid beta plaques (protein deposits in the brain’s grey matter), Alzheimer’s permanently alters a person’s memory and cognitive functioning. Unlike other Alzheimer’s treatments that work to manage symptoms, Leqembi was shown, over the course of its clinical trials, to slow amyloid plaque buildup in the brain. It’s the first such Alzheimer’s treatment to have shown clinical benefit, according to Teresa Buracchio, the acting director of the Office of Neuroscience for the FDA’s Center for Drug Evaluation and Research.
Just before Leqembi hit the market, researchers at the University of Pittsburgh and the University of Gothenburg in Sweden made a groundbreaking discovery about astrocytes, a type of star-shaped brain cell that controls a number of different brain functions. Astrocytes may become “reactive”—undergoing physical or chemical changes—in response to problems in the brain. While amyloid plaques are central to Alzheimer’s pathology, their existence alone does not reliably predict the onset of the disease. However, researchers found that the combined presence of amyloid plaques with reactive astrocytes more dependably indicates a patient’s risk of developing Alzheimers.
The study’s results argue that the double screening for the presence of amyloid plaques in addition to reactive astrocytes is the most appropriate method to assess patients’ risk of developing the disease. In tandem with Leqembi, this breakthrough discovery in the underlying cause of Alzheimer’s development has rapidly sparked the beginning of a new era for those suffering from the disease.
These six watershed medical advancements have not only pushed the boundaries of science and imagination but have also offered hope for countless patients in need. With each discovery, we continue to progress into the realm of the unknown, inching closer to a healthier future, in which the barriers of disease are challenged and overcome. The remarkable medical advancements of 2023 serve as a testament to the knowledge and dedication of our medical professionals, researchers, and scientists worldwide.